What Are the Risks Associated with Dental Implants?
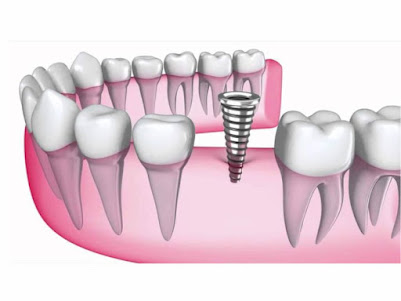
Dental implants are a popular and highly effective solution for replacing missing teeth. They offer a permanent and natural-looking alternative to dentures and bridges, providing long-term benefits such as improved oral function, aesthetics, and bone health. However, like any surgical procedure, dental implants come with potential risks and complications. While the success rate of dental implants is high—around 95%—it's essential to understand the risks involved to make an informed decision.
This article provides an in-depth look at the various risks associated with dental implants, including surgical complications, infection, implant failure, and long-term issues.
1. Infection at the Implant Site
One of the most common risks associated with dental implants is infection at the implant site. This can occur during or after the surgery if bacteria enter the surgical area. Symptoms of infection may include redness, swelling, pain, and discharge. In severe cases, the infection can spread to the surrounding tissues or even the bone (osteomyelitis), potentially leading to implant failure.
To minimize the risk of infection, your dentist or oral surgeon will likely prescribe antibiotics and provide detailed post-operative care instructions. Good oral hygiene is crucial during the healing process, as it helps prevent bacterial buildup around the implant.
2. Nerve Damage
Nerve damage is a potential complication, especially when the implant is placed in the lower jaw, where important nerves run close to the bone. If the implant is placed too close to the nerves, it can lead to numbness, tingling, or pain in the gums, lips, chin, or even the tongue.
In some cases, this nerve damage may be temporary and resolve on its own as the tissues heal, but in other cases, it can be permanent. To prevent this risk, a dentist will use advanced imaging techniques such as 3D X-rays or CT scans to plan the precise placement of the implant, avoiding contact with vital structures.
3. Implant Failure
While dental implants boast a high success rate, there is always the risk of implant failure. This occurs when the implant does not properly integrate with the surrounding bone—a process known as osseointegration. Without proper fusion between the implant and the bone, the implant may become loose or dislodged.
Factors that can contribute to implant failure include:
Insufficient bone density: The jawbone must be strong enough to support the implant.
Poor oral hygiene: Inadequate cleaning around the implant can lead to plaque buildup, infection, and failure.
Smoking: Smoking negatively affects healing and increases the likelihood of implant failure.
Bruxism (teeth grinding): Constant pressure on the implant from teeth grinding can cause it to shift or fail.
If an implant fails, it may need to be removed, and the area might require bone grafting before attempting a new implant.
4. Sinus Problems
In cases where dental implants are placed in the upper jaw, there is a risk of sinus problems if the implant extends into the sinus cavity. The proximity of the upper jaw to the sinus is a critical factor, and improper placement of the implant can lead to sinusitis, chronic discomfort, or even infection of the sinuses.
Before implant placement in the upper jaw, the dentist may recommend a sinus lift—a procedure that increases the amount of bone in the upper jaw to ensure proper placement without affecting the sinus cavity.
5. Bone Loss Around the Implant
Bone loss around the implant, also known as peri-implantitis, is a condition where the bone that supports the implant starts to degrade. This can occur if bacteria accumulate around the implant, leading to inflammation and gradual bone loss.
In the early stages, peri-implantitis may be asymptomatic, but as it progresses, symptoms such as bleeding, pain, and swelling may develop. If not addressed, it can eventually result in implant failure. Regular dental check-ups and excellent oral hygiene are essential to monitor for signs of peri-implantitis and prevent its progression.
6. Overloading the Implant
Overloading happens when the dental implant is subjected to excessive force too soon after surgery. This may occur if the crown or prosthetic tooth is placed before the implant has fully integrated with the bone. The bone around the implant needs time to heal and bond with the implant, and placing too much pressure on it prematurely can cause the implant to become loose or shift out of position.
To prevent overloading, dentists typically wait a few months after implant surgery before placing the final crown or bridge. This allows ample time for osseointegration, reducing the risk of implant failure.
7. Allergic Reaction to Materials
Dental implants are typically made from titanium or titanium alloys, which are biocompatible and rarely cause allergic reactions. However, in rare cases, some patients may experience an allergic reaction to the metals used in the implant. Symptoms of an allergic reaction may include itching, swelling, and redness around the implant site.
If you have a known allergy to metals, it is essential to inform your dentist beforehand. In such cases, alternative materials, such as zirconia, may be used for the implant.
8. Blood Vessel Damage
Blood vessel damage is another potential risk during implant surgery, particularly if the implant is placed near large blood vessels. If a blood vessel is accidentally punctured, it can result in excessive bleeding, bruising, or hematoma (a collection of blood outside the blood vessels). In most cases, the bleeding will subside on its own, but severe cases may require medical intervention.
Dentists use detailed imaging to avoid major blood vessels during the surgery, minimizing the risk of this complication.
9. Anesthesia Complications
Dental implant surgery is usually performed under local anesthesia, though sedation or general anesthesia may be used in more complex cases. Anesthesia-related risks are generally low but can include allergic reactions, respiratory problems, or, in rare cases, cardiovascular issues.
Patients should discuss their medical history, including any allergies or previous reactions to anesthesia, with their dentist or oral surgeon before the procedure.
Conclusion
Dental implants are a reliable and long-lasting solution for tooth replacement, offering numerous benefits for patients. However, like any surgical procedure, they come with certain risks. While the vast majority of dental implants are successful, it’s important to be aware of potential complications such as infection, nerve damage, and implant failure.
By choosing an experienced dental professional, maintaining good oral hygiene, and following post-operative care instructions closely, you can significantly reduce the likelihood of complications and enjoy the long-term benefits of your dental implants.
If you're considering dental implants, consult with your dentist to evaluate your individual risk factors and determine the best course of action for your oral health.


Comments
Post a Comment